What is an Annular Bulge?

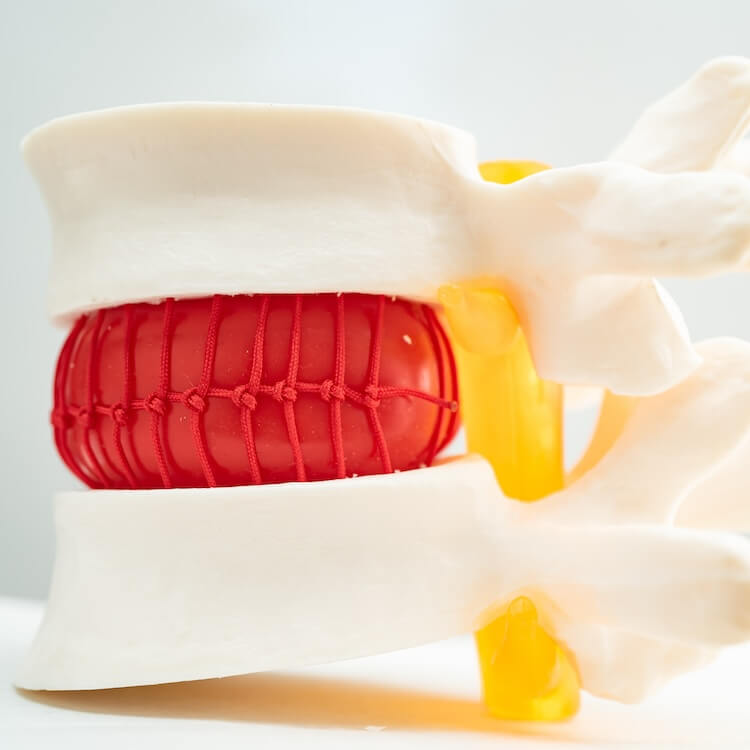
An annular bulge happens when the outer part of the disc, called the annulus fibrosus, begins to bulge outward. This occurs without the inner portion of the disc, known as the nucleus pulposus, breaking through the outer layer. The disc remains intact, but the pressure it exerts on surrounding structures can lead to pain and discomfort.
Unlike a herniated disc, where the disc material breaks through the outer layer, an annular bulge keeps the inner material contained. However, both conditions can cause similar symptoms, depending on how much the disc is pressing on the nearby nerves.
Understanding Bulging Discs
Bulging discs are one of the more common spinal issues, particularly as people age. The condition occurs when the outer layer of an intervertebral disc starts to weaken, leading to a bulging disc. This bulge can press on nearby spinal nerves, causing symptoms that range from mild discomfort to severe pain.
While not as severe as a herniated disc, a bulging disc can still lead to significant issues if left untreated. The bulge may press against the spinal cord, potentially causing nerve compression and discomfort that can extend to other parts of the body. Bulging disc symptoms often include back pain, muscle weakness, and difficulty with certain movements like bending or lifting.
How Do Bulging Discs Occur?
Bulging discs occur most frequently as part of the natural aging process. Over time, the outer layers of the discs lose elasticity, becoming less able to contain the inner portion of the disc, also known as the nucleus pulposus. This results in the disc slowly pushing outward, which may eventually lead to a bulge.
In younger individuals, bulging discs can develop due to factors such as heavy lifting, traumatic injury, or poor posture. Repeated strain on the spinal column can weaken the disc and lead to its outward bulge, making prevention through proper lifting techniques critical.
Causes and Risk Factors of a Bulging Disc
A bulging disc can develop gradually or as a result of injury. One common cause is disc degeneration, which occurs as part of the natural aging process. Over time, the intervertebral discs in the spine lose their flexibility and strength. This leads to a weakened outer layer of the disc, making it more prone to bulging.
Individuals who engage in heavy lifting, or those with poor posture, are also more likely to develop bulging or herniated discs. Wear and tear on the disc from repetitive movements, especially in the lumbar spine, puts stress on the annulus fibrosus, the thick outer layer of the disc. Over time, this can lead to a disc bulge.
While bulging discs may not always cause symptoms, they can lead to complications if they press against nerves. A compressed nerve can lead to pain symptoms, muscle weakness, and even difficulty walking. In some cases, a pinched nerve from the bulging disc may cause pain to radiate into the legs or arms, depending on the location of the bulge.
Symptoms of Bulging or Herniated Discs
The symptoms of bulging discs vary depending on the severity and location of the bulge. Common bulging disc symptoms include back pain, numbness, and tingling. If the disc is pressing on the sciatic nerve, the pain may radiate down the legs, causing discomfort in the lower body.
A herniated disc, on the other hand, often causes more intense symptoms. In a herniated disc, the inner layer of the disc pushes through a tear in the outer layer, often leading to more severe pain and nerve irritation. Annular tears can occur when the disc's annulus fibrosus is damaged, causing the disc pain to worsen. Symptoms can also include muscle spasms and loss of flexibility.
Patients with lumbar disc herniation may experience pain radiating into the legs, while those with a herniation in the cervical spine may feel discomfort in the neck and arms. Neck pain, caused by either a bulging or herniated disc, is often due to the disc pressing on the nerve roots in the neck area. This pain can be accompanied by stiffness, limited mobility, and, in severe cases, loss of leg muscles or arm strength.
Diagnosing Bulging or Herniated Discs
To properly diagnose a bulging disc or herniated disc, a physician will perform a thorough physical examination and review the patient’s medical history. The doctor may also order imaging tests such as a CT scan or MRI to get a detailed view of the spine. These tests can identify the presence of disc herniation, disc extrusion, or annular fissures.
A bulging disc may not always be symptomatic, but if there is nerve compression, it can cause significant discomfort. A CT scan can reveal the exact location of the bulge or herniation and determine if it’s pressing against the spinal cord or nerve roots.
Once the diagnosis is confirmed, the physician will evaluate the severity of the damaged disc and the level of nerve compression. This helps in determining the best bulging disc treatment options, which could range from conservative approaches to surgical interventions.
The Role of Disc Degeneration in Bulging Discs
Disc degeneration is a major contributing factor to the development of a bulging disc. As the intervertebral discs naturally age, they begin to lose their elasticity and hydration, making them more prone to bulging or disc herniation. This degeneration process is often a result of wear and tear on the vertebral discs, which function as cushions between the bones in the spine, providing shock absorption.
Over time, the outer layers of the disc—known as the annulus fibrosus—can weaken, leading to annular tears or annular fissures. These small cracks in the disc’s surface can cause the disc to bulge outward and press on nearby structures like the spinal cord or nerve roots. While disc degeneration is often part of the natural aging process, other factors such as injury, poor posture, or repetitive strain can accelerate this process, leading to a disc bulge.
Symptoms of a Bulging Disc and Annular Tear
Patients with a bulging disc or annular tear may experience a range of symptoms, from mild discomfort to severe pain. The symptoms largely depend on the location of the disc bulge and the degree of pressure it places on the spinal cord or surrounding nerves. Annular tears often lead to localized pain in the back, while more severe cases, such as when a disc bulge compresses the spinal nerves, can cause radiating pain, numbness, and difficulty walking.
The pain from a bulging disc may be felt after sitting or standing for long periods, or during activities that involve bending or lifting. In more advanced cases, patients might experience muscle weakness, tingling, or even trouble walking due to nerve compression. For those dealing with degenerative disc disease, these symptoms can become more pronounced as the discs continue to deteriorate over time.
Conservative Treatments for Bulging Discs
The good news is that most cases of bulging discs can be treated with conservative treatments. These approaches focus on relieving pain and improving function without the need for surgery. Physical therapy plays a significant role in treating bulging disc symptoms, as it helps strengthen the muscles that support the spine and improve flexibility. A physical therapist will often guide patients through a series of exercises aimed at reducing pressure on the intervertebral discs and preventing further injury.
In addition to physical therapy, other non-invasive methods such as anti-inflammatory medications and muscle relaxants can be used to manage pain and reduce inflammation. These medications can help ease the discomfort caused by the bulging disc pressing against the spinal cord or nerves. However, it's important to combine medication with physical therapy for long-term relief and recovery.
Rest and avoiding activities that place strain on the spine are also crucial during recovery. While rest is important, it's equally essential to avoid prolonged inactivity, as this can weaken the muscles around the spine, making the problem worse. Patients are often encouraged to remain active with low-impact exercises, as guided by their physical therapist.
Physical Therapy and Long-Term Management
Physical therapy is not only useful for immediate relief but also plays a critical role in the long-term management of bulging discs and other spine-related issues. Strengthening the core and back muscles helps provide stability to the spine, reducing the risk of further disc degeneration or herniation. Patients may be taught how to properly lift objects, improve their posture, and perform stretches that enhance flexibility.
Exercises aimed at increasing flexibility and stability can help reduce the risk of future disc injuries. Physical therapists often incorporate targeted exercises that focus on the core, glutes, and back muscles. By stabilizing the spine, these muscles provide better support to the vertebral discs, lowering the chances of recurring issues.
Minimally Invasive Procedures for Bulging Discs
In cases where conservative treatments do not adequately reduce pain or restore function, minimally invasive procedures may be necessary. These procedures are often performed to alleviate pressure on the spinal cord or nerve roots caused by the bulging or herniated disc.
One common option is minimally invasive spine surgery, where a surgeon makes a small incision and uses specialized tools to remove part of the damaged disc. This can help relieve the pressure on the nerves, reducing pain and improving mobility. Because the procedure is minimally invasive, patients typically experience a shorter recovery time and fewer complications compared to traditional open surgery.
Another treatment option includes steroid injections around the bulging disc, which can reduce inflammation and provide relief for several months. This method, combined with physical therapy, can help patients manage their symptoms without the need for more invasive treatments.
The Importance of Early Treatment for Annular Tears
Annular tears are small tears in the outer layer of the disc, and if left untreated, they can lead to more serious conditions such as a full herniated disc. Early detection and treatment are essential to prevent these tears from worsening. Symptoms of annular tears can include localized disc pain, as well as radiating pain that spreads into the legs or arms if the tear presses on nearby nerves.
While minor annular tears can sometimes heal with rest and conservative treatments, larger tears may require more active interventions, such as minimally invasive procedures or injections to reduce pain. Managing these tears early on with physical therapy and proper body mechanics can help avoid further damage and ensure a quicker recovery.
Managing Pain and Preventing Future Injuries
Managing pain from a bulging disc or annular tear is essential for maintaining mobility and quality of life. Medications such as anti-inflammatory drugs can help, but long-term pain management often involves a combination of treatments. Engaging in a physical therapy program is one of the best ways to strengthen the back and reduce strain on the spine.
Learning and adhering to proper lifting techniques is another critical component of preventing further disc degeneration. Avoiding repetitive bending, twisting, and lifting heavy objects improperly can help reduce the risk of aggravating a bulging disc or developing new disc tears.
For those with chronic disc problems, maintaining a healthy weight is also key, as extra weight can put additional stress on the vertebral discs. By staying active and following a consistent exercise routine, many individuals can prevent recurring disc issues and live a more comfortable, pain-free life.
Dr. Abdul Baker - An Expert Neurosurgeon in Texas
Every neurosurgery has its complications; thus, a patient must choose the best neurosurgeon for himself. Dr. Abdul Baker is one of the most experienced and qualified neurosurgeons in Texas, treating patients for more than 16 years. People in Sherman, Plano, and nearby areas trust him for every kind of neurosurgery due to his surgical procedures’ 100% success rate. You may visit him if you need any consultancy or treatment regarding your brain and spine disorders.

Dr. Baker specializes in neurosurgery, neurosurgical spine surgery, neurotrauma, brain tumors, spinal tumors, and peripheral nerve damage treatment.