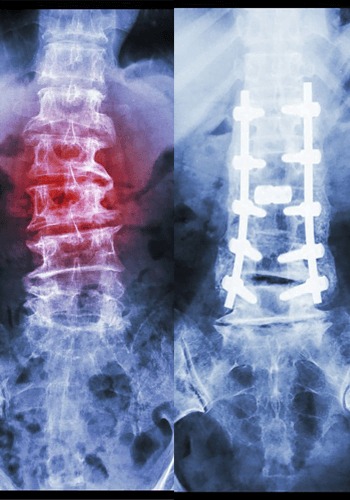
Spinal Reconstruction Surgery
Successful reconstructive spine surgery requires a highly experienced and qualified surgeon.
Complex Spinal Reconstruction is only used to treat the most severe spine problems and should be performed by a highly trained, experienced surgeon.
Spine surgery or reconstructive spine surgery is only recommended when traditional therapy has failed and minimally invasive surgery will not solve the problem.
Patients who are candidates for reconstructive spine surgery generally suffer from complex spine conditions resulting from scoliosis, spinal deformities, fractures, tumors, or severe degenerative disc disorder.
Reconstructive spine surgery should only be performed by the most experienced spine surgeon because of the unique pathology of each case. Compared to minimally invasive surgery, complex spine surgery has much greater variability during the procedure creating a higher risk of complications.
Dr Baker's many years of experience and elite level of expertise make him the perfect choice for spinal reconstruction surgery.
Request an Appointment
Is Spinal Reconstruction Surgery right for me?
Although only your doctor can tell you if Spinal Reconstruction Surgery is the right treatment plan for you, you might be a qualifying candidate if:
- You are experiencing pain from scoliosis, severe degenerative disc disease, spinal deformities, or spinal tumors
- You suffer from co-occurring disorders such as scoliosis paired with degenerative disc disease
- You have tried other treatment options like (but not limited to) physical therapy, bracing, or even minimally invasive surgery without success
- Your diagnosis calls for surgery across more than 3 spinal segments
- You have failed back surgery syndrome from previous spine surgery and your pain or symptoms are worsening
Anterior Cervical Discectomy and Fusion

Anterior Cervical Discectomy and Fusion
ACDF or Anterior Cervical Discectomy and Fusion is a minimally invasive neck procedure where a degenerative or herniated disc is removed from the neck. After the disc is removed, a graft is used to fuse the two vertebrae above and below the damaged disc.
Explaining the ACDF Acronym
A stands for Anterior – This procedure is done from the front or anterior part of the body. In ACDF surgery, a small, minimally-invasive incision is made in the front of the neck.
C stands for Cervical – The cervical spine consists of the top 7 vertebrae (C1-C7) which is most commonly referred to as the neck.
D stands for Discectomy – A discectomy means to cut out, or remove the disc. A discectomy can be performed anywhere on the spine.
F stands for Fusion – The final stage of the procedure involves inserting a bone graft to replace the empty space caused by the missing disc and fusing the two vertebrae together for stability.
Frequently Asked Questions about
Spinal Reconstruction Surgery
How long is the Recovery Time for Reconstructive Spine Surgery?
Although the recovery time will depend on the extent of your surgery and your general health before the procedure, you should expect to need some downtime and rest immediately following the surgery.
Reconstructive Spine Surgery is usually done in a hospital rather than a surgery center because some procedures can require a few days stay. Patients generally feel some pain after the surgery and during recovery. The pain will subside and most patients report happiness with the results within just a few short months.
What Considerations Should be Taken in the Healing Process?
What are Some of the Possible Complications from Anterior Cervical Discectomy and Fusion?

Dr. Baker specializes in neurosurgery, neurosurgical spine surgery, neurotrauma, brain tumors, spinal tumors, and peripheral nerve damage treatment.