Artificial Disc Replacement
When it comes to minimally invasive procedure, the evolution of medical technology has fundamentally transformed the artificial disc replacement surgery procedure, and has helped improve and enhance outcomes for patients, shorten recovery time and hospital stay and help increase the quality of life for patients.
The advent of artificial disc replacement surgery helped neurosurgeons address a wide range of patient issues and offer hope for those suffering from conditions such as lumbar disc herniation, damaged discs and diseases of the cervical and lumbar spine.
Understanding the Spine
The spine is vital in the human body, it is what facilitates free and flexible movement, helping you bend and move.
In addition to providing the support and structure to do this, the spine is responsible for the protection of the spinal cord, which is a vital part of your central nervous system and responsible for relaying signals from your brain to the rest of your body.
Understanding the anatomy and function of the spine often helps patients suffering from back pain come to a more fully informed decision when it comes to treatment choices.
Request an Appointment
The Segments of the Spine
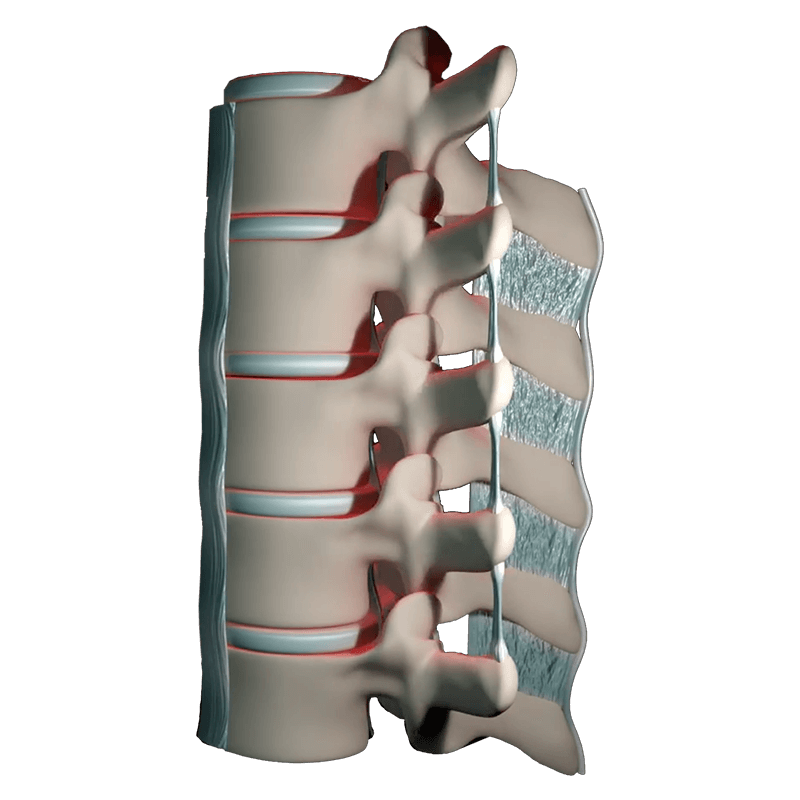
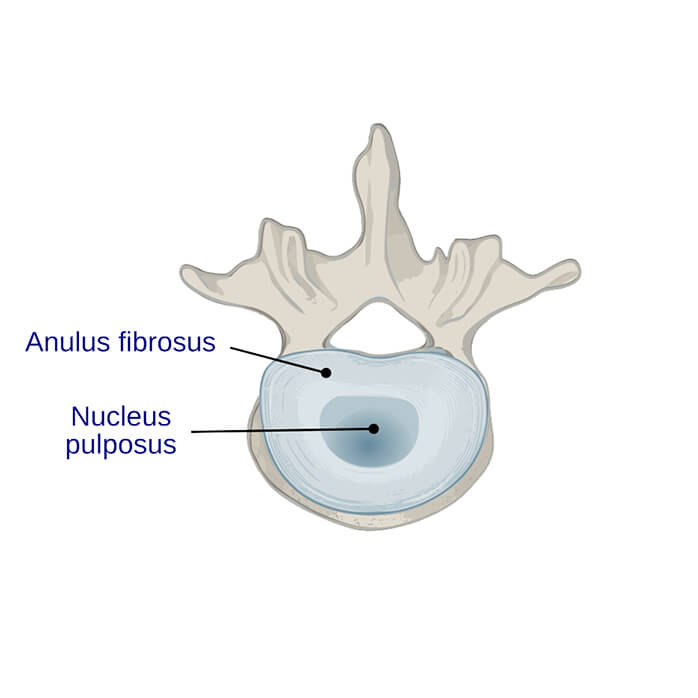
The spine is made of of 24 segments, which are called vertebrae, which are separated by softer disc-like cushions which are made up of an outer ring of thick fibrous cartilage known as annulus fibrosus and an inner portion of softer gelatinous matter called nucleus pulposus.
The spinal column itself is separated into distinct sections, these are called the cervical, thoracic, lumbar, sacrum and coccyx.
The Cervical Spine
The cervical spine consists of the top 7 discs, often referred to as C1 to C7, these are responsible for supporting the weight of the head and providing its range of motion.
These vertebrae are the reason why you can turn your head, nod, look up and down, it also protects the spinal cord at one of the most vital points, damage to the spinal cord in the cervical spine can result in quadriplegia or tetraplegia including potential respiratory issues, bladder and bowel control.

The Thoracic Spine
The Lumbar Spine
The thoracic spine or upper back are attached to the rib cage, this somewhat limits the range of motion compared to the lumbar and cervical region, however it is responsible for protecting the vital organs that are located in the chest area such as the heart and lungs.
The lumbar spine bears the majority of the body's weight and is the one that is most often under pressure when lifting objects, standing and it provides important flexibility for bending, twisting and leaning whilst stabilising and supporting the abdomen and trunk area.
Sacrum and Coccyx or Coccygeal Region
The vertebrae in the sacrum are fused and are responsible for connecting the spine to the pelvis or hips. The sacrum forms the back portion of the pelvis and this supports the weight of the upper body when standing or sitting.
The coccyx is also made up of fused coccygeal vertebrae and provides the attachment points for the Levator Ani muscles which connect the pelvic organs, the Coccygeus muscles which form part of the pelvic floor, the Sacroccygeal ligaments and several other muscles int he lower back and buttocks. These muscles largely contribute to various movements including hip extension and trunk stabilisation.
When Artificial Disc Replacement Surgery is Needed?
Artificial disc replacement surgery spans the cervical, thoracic, lumbar and sacral regions of the spine and is a treatment option for a range of conditions and functional limitations. In general, such an intervention has the aim of reducing pain, enhancing quality of life and promoting natural motion and flexibility.
Cervical disc replacement surgery can be required in cases where disc degeneration has led to neck pain, radiating arm pain or other neurological symptoms.
Thoracic disc replacement surgery can be required in cases where the patient is suffering from severe thoracic pain which can be caused by discogenic issues.
Lumbar disc replacement surgery is generally the most common one that patients present with, it is one of the most common spine surgery treatments and can be used in cases of lumbar degenerative disc disease. Lumbar disc degeneration can result in chronic low back pain and leg pain.
Patients with significant facet joint disease or degenerated discs can benefit from lumber total disc arthroplasty. Lumbar disc replacement surgery can also be used in cases of chronic back pain, usually only after all conservative treatment options fail to provide relief.
How Artificial Disc Replacement Surgery Works?
Artificial disc replacement surgery is a transformative solution for patients grappling with degenerative disc disease, discogenic low back pain, or spinal stenosis.
It offers an alternative to traditional spinal fusion surgery, which restricts motion in the affected area. Artificial disc replacement focuses on preserving spinal mobility and function, typically utilizing lumbar artificial disc replacements.
Before the surgery, patients undergo a comprehensive evaluation, including magnetic resonance imaging (MRI) to assess the condition of the affected disc and surrounding structures. This step allows for precise planning and customization of the procedure, ensuring optimal outcomes. Magnetic Resonance Imaging, along with x-rays, helps in evaluating the blood vessels' proximity and confirming the suitability of artificial disc replacement.
During artificial disc replacement surgery, the damaged lumbar disc is replaced with a high-quality artificial disc made from medical-grade cobalt-chromium or similar materials. The artificial disk design mimics natural discs, the disc prosthesis provides flexibility and acting as a mechanical shock absorber. This approach allows for a safer procedure that minimizes trauma to surrounding tissues, resulting in less postoperative pain.
Post-surgery, patients often benefit from physical therapy and basic exercises to aid in recovery and regain strength. Artificial disc replacement surgery's safety and effectiveness are supported by a wealth of clinical research and studies, showcasing its superiority in preserving spinal function and mitigating pain compared to traditional lumbar fusion techniques.
Treatments such as Lumbar artificial disc replacement, guided by advanced imaging like MRI, represents a safe procedure for those dealing with degenerative disc disease, discogenic low back pain, or spinal stenosis. By focusing on spinal motion preservation, this innovative approach offers patients an opportunity to regain their quality of life and mobility while minimizing postoperative discomfort.
What Is the Purpose of Artificial Disk Replacement Surgery?
As we age, our vertebral discs naturally undergo compression and bulging. By the age of 60, most individuals will have experienced these changes to some extent. Nevertheless, the perplexing question that continues to puzzle healthcare providers is why certain patients endure more pronounced symptoms associated with cervical disc degeneration than others.
With locations in Sherman and Plano in Texas, Dr. Baker stands out as a leading expert in disc replacement surgery. He specializes in providing top-tier care to address the common issue of cervical disc degeneration, a condition marked by the loss of space between cervical vertebrae due to wear and tear.

Cervical disks, over time, tend to collapse and bulge as part of the natural aging process. This phenomenon typically manifests in most people by the age of 60. The exact reasons for the variability in symptoms among individuals with cervical disc degeneration remain a medical enigma.
Symptoms may include:
Pain & Stiffness in the neck
Continuous Back Pain
Headaches
Pain that travels into shoulders & arms
Weakness of shoulders, arms, hands & legs
Numbness or pinching in arms & legs
Reduced reflexes in the knee & ankle
How is a Cervical Disc Replaced?
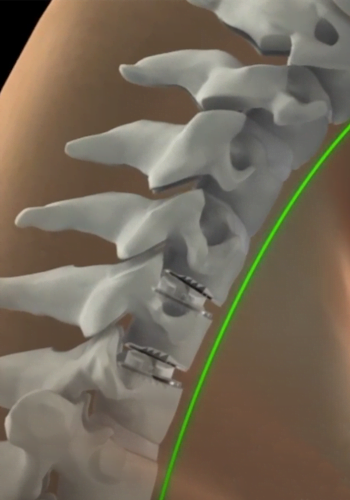
The use of an artificial disc to replace your natural cervical disc is a novel FDA-approved procedure. A diseased cervical disc is removed and then replaced with an artificial disc during cervical disk replacement surgery.
Prior to the availability of this procedure, the surgery was done by removing the affected disc. The vertebrae above and below were fused to prevent motion. Nowadays, the following steps are involved in artificial disk replacement surgery.
- An incision of 1-2 inches is made on the throat area to remove the diseased cervical disk.
- The artificial disk is replaced in place of the removed cervical disk.
- Two metal plates of the disk are anchored with the upper and lower parts of the joints at the surgical spot.
- The incision is closed with the help of absorbable stitches under the skin.
A rigid or soft collar is also put on the neck at the end of the surgery for restricted movement.
Frequently Asked Questions about
Artificial Disc Replacement
What are the Benefits of Cervical / Artificial Disc Replacement?
Disk replacement surgery may allow more movement and create less stress on your remaining vertebrae than traditional cervical disk surgery. Here are the most common benefits of artificial spine and lumbar disk replacement surgery.
- Cervical disk replacement helps maintain the full range of neck motion.
- This surgery decreases the possibility of degeneration in the cervical spine’s adjacent segments.
- It minimizes the risks associated with bone grafts.
- Most patients are able to resume full physical activity in three months, including jogging or some exercise.
- This surgery has a shorter recovery time so that the patients can resume their normal daily activities after one month of the surgery.
- Lumbar disk replacement reduces discogenic back pain and restores normal disk height.
Are there any Risks or Issues with Artificial Disc Replacement Surgery?
What is the difference between Artificial Disc Replacement and Fusion Surgery?

Dr. Baker specializes in neurosurgery, neurosurgical spine surgery, neurotrauma, brain tumors, spinal tumors, and peripheral nerve damage treatment.