Platelet Rich Plasma Therapy Arthritis Treatment

Platelet-rich plasma (PRP) therapy has gained attention as a promising treatment for arthritis, offering effective relief for individuals dealing with joint pain and limited mobility. By harnessing the body’s natural healing process, PRP therapy uses the patient’s own blood to promote tissue repair and reduce inflammation.
The process involves drawing a blood sample, which is then processed to concentrate the platelets and growth factors vital for healing. Once prepared, the platelet-rich plasma is injected directly into the affected joint, such as the knee, to help alleviate the symptoms of arthritis.
PRP therapy is particularly effective for knee osteoarthritis, a condition marked by the gradual breakdown of cartilage in the joint, leading to pain and stiffness. PRP injections have shown significant promise in not only reducing pain but also improving knee function and slowing the degenerative process. For those interested in alternative regenerative treatments, stem cell therapy for arthritis offers another potential option worth exploring.
Unlike traditional treatments like corticosteroid injections or hyaluronic acid, PRP therapy enhances the body’s own regenerative capabilities, making it an appealing choice for patients seeking long-term solutions.
The increasing popularity of platelet-rich plasma therapy for arthritis is supported by growing clinical evidence and patient success stories. With minimal side effects and the potential for lasting relief, PRP therapy is becoming a go-to treatment for those looking to manage arthritis symptoms and improve their quality of life without resorting to surgery or more invasive procedures.
How Does Platelet-Rich Plasma Therapy Work?
Platelet-rich plasma (PRP) therapy is a regenerative treatment that relies on the body's natural healing process. It begins with drawing a small sample of the patient’s blood, which is then placed in a centrifuge to separate its components.
The centrifuge spins the blood at high speeds, isolating the platelet-rich plasma, which is dense with growth factors and proteins that play a key role in tissue repair. These growth factors help to stimulate cellular regeneration, reduce inflammation, and accelerate healing in damaged tissues.

Once the platelet-rich plasma is prepared, it is injected directly into the affected joint, such as the knee in cases of knee osteoarthritis. The goal of these PRP injections is to deliver a high concentration of healing factors directly to the damaged area, thereby enhancing the body’s ability to repair cartilage, reduce pain, and improve joint function.
PRP works by triggering a local inflammatory response that promotes the healing of soft tissues, which is particularly beneficial in degenerative conditions like arthritis.
The process is relatively straightforward and is performed on an outpatient basis. The injection itself typically takes less than an hour, and most patients experience minimal discomfort. While the healing process is gradual, many patients begin to notice improvements in pain levels and joint mobility within weeks of the treatment.
PRP therapy offers a natural, non-surgical approach to treating arthritis, making it a preferred option for those who want to avoid more invasive procedures.
Research and clinical studies have supported the effectiveness of PRP therapy in treating osteoarthritis and other joint-related conditions. The use of autologous platelet-rich plasma—meaning the patient’s own blood—is key to minimizing risks like allergic reactions and maximizing the body’s ability to heal itself. PRP treatment continues to gain recognition in the fields of orthopaedic surgery and regenerative medicine as a powerful tool in managing arthritis and promoting long-term joint health.
The Role of Platelet-Rich Plasma in Treating Osteoarthritis
Platelet-rich plasma (PRP) therapy has become a promising option for treating osteoarthritis, particularly in joints like the knee, where cartilage degradation leads to pain, stiffness, and reduced mobility. Knee osteoarthritis, a common condition in older adults, results from the gradual breakdown of articular cartilage, which cushions the bones in the joint. PRP injections aim to address this issue by delivering concentrated growth factors directly to the affected joint, stimulating cartilage repair, reducing inflammation, and enhancing overall joint function.
Unlike traditional treatments such as corticosteroids or hyaluronic acid, which primarily focus on symptom relief, PRP therapy targets the underlying degenerative process. The growth factors in platelet-rich plasma are believed to promote the healing of damaged cartilage and improve the quality of the remaining tissue. This makes PRP therapy particularly beneficial for those with symptomatic knee osteoarthritis who have not responded well to other treatments.
Clinical studies and randomized trials have shown that PRP therapy can lead to significant improvements in pain levels and knee function, allowing patients to engage in physical activities with less discomfort. The treatment is especially valuable for individuals who are not yet candidates for joint replacement surgery but need an effective solution to manage their arthritis symptoms. By leveraging the body’s natural healing mechanisms, PRP therapy offers a regenerative approach that helps slow the progression of osteoarthritis, giving patients a better quality of life.
Overall, platelet-rich plasma therapy is emerging as a key tool in managing osteoarthritis, with many patients experiencing reduced pain, improved mobility, and a delay in the need for more invasive interventions like surgery.
PRP Injections: What to Expect?
The process of receiving platelet-rich plasma (PRP) injections for arthritis is straightforward and minimally invasive. It begins with a blood sample drawn from the patient, typically from the arm. This blood sample is then placed in a centrifuge, which spins rapidly to separate the blood components. The goal is to isolate the platelet-rich plasma, which contains concentrated growth factors that are crucial for promoting healing and reducing inflammation.
Once the PRP is prepared, it is injected directly into the affected joint, such as the knee in cases of knee osteoarthritis. The injection is carefully administered by a medical professional, often guided by ultrasound to ensure precise placement of the PRP in the area needing treatment. The entire procedure usually takes less than an hour and is performed on an outpatient basis, allowing patients to return home the same day.
While the injection itself can cause mild discomfort, most patients tolerate it well. Some experience temporary pain, swelling, or stiffness at the injection site, which typically subsides within a few days. Unlike other treatments like corticosteroids or hyaluronic acid injections, PRP therapy is designed to enhance the body’s natural healing process by delivering a high concentration of growth factors where they are needed most.
Patients often require multiple injections over several weeks or months to achieve optimal results, depending on the severity of their arthritis. Following the procedure, patients are advised to avoid strenuous activities for a short period but can gradually return to their regular routines. PRP injections offer a non-surgical alternative for treating osteoarthritis, providing pain relief and improved joint function without the extended recovery times associated with more invasive procedures.
The Science Behind Platelet-Rich Plasma Therapy
Platelet-rich plasma (PRP) therapy leverages the body’s natural healing process to treat conditions like knee osteoarthritis and other degenerative joint issues. This treatment begins with drawing a blood sample from the patient. The blood is then placed in a centrifuge, where it is spun at high speeds to separate the components. The goal is to isolate the platelet-rich plasma, which contains concentrated growth factors, white blood cells, and other key elements that promote tissue repair. The PRP is then injected directly into the affected joint, targeting areas where cartilage has been damaged, and inflammation is present.
How PRP Injections Work for Symptomatic Knee Osteoarthritis
PRP injections work by delivering a high concentration of growth factors directly into the affected joint. These growth factors accelerate the healing process by promoting the regeneration of articular cartilage and enhancing joint function. In cases of symptomatic knee osteoarthritis, where the cartilage is wearing away, PRP therapy helps reduce pain, improve knee function, and slow the degenerative process. This is particularly beneficial for patients who are not yet candidates for more invasive procedures like orthopaedic surgery or stem cell therapy.
Platelet-Rich Plasma vs. Traditional Arthritis Treatments
One of the reasons platelet-rich plasma therapy has gained popularity is because it offers an alternative to traditional treatments like corticosteroid injections, hyaluronic acid, and physical therapy. While these treatments can provide temporary relief, they do not address the underlying pathologic processes that lead to joint deterioration. PRP treatment, on the other hand, focuses on long-term healing by enhancing the body’s natural ability to repair itself. For example, unlike hyaluronic acid injections that primarily lubricate the joint, PRP injections target the root causes of knee osteoarthritis by promoting cartilage repair and reducing inflammation.
Clinical Outcomes and the Role of Randomized Controlled Trials
The effectiveness of PRP therapy has been demonstrated through multiple randomized controlled trials and clinical studies. These trials have shown that platelet-rich plasma injections can provide significant improvement in pain relief and joint function for patients with knee osteoarthritis and other musculoskeletal conditions. Clinical outcomes indicate that PRP therapy offers better long-term results compared to placebo treatments and even some conventional therapies. Research published in journals like J Sports Med and Clin J Sport Med highlights the role of platelet-rich plasma PRP in treating joint conditions, with patients experiencing functional improvement and reduced pain.
PRP Preparation Methods and Their Impact on Results
The effectiveness of PRP therapy can vary depending on the PRP preparation methods used. The concentration of platelets and the inclusion of white blood cells or red blood cells can affect the treatment’s efficacy. Autologous platelet-rich plasma, which is derived from the patient’s own blood, is the most common form used in PRP therapy. Different techniques for processing whole blood can result in variations in platelet concentration, impacting the overall success of the treatment. Medical professionals must carefully consider these factors when administering PRP injections to ensure optimal clinical outcomes.
PRP Therapy in Regenerative Medicine and Sports Medicine
PRP therapy is increasingly recognized in both regenerative medicine and sports medicine. In addition to treating knee osteoarthritis, PRP injections are widely used for soft tissue injuries like tennis elbow, ligament sprains, and tendonitis. The ability of PRP to promote tissue repair and accelerate healing has made it a go-to treatment for athletes and individuals with sports injuries. In the field of orthopedic surgery, PRP is often used alongside other therapies like stem cell treatment to enhance recovery from cartilage defects and joint injuries.
PRP Treatment for Multiple Conditions and the Future of Research
As research in the field of PRP therapy continues to grow, new applications and treatment strategies are emerging. PRP is now being explored as an effective treatment for a variety of musculoskeletal conditions, including shoulder injuries, hip osteoarthritis, and even spinal issues. New research and basic science evidence continue to refine how PRP works, leading to improvements in clinical outcomes and paving the way for even broader use in treating chronic pain and joint dysfunction. As more clinical studies are conducted, the role of PRP therapy in managing degenerative processes and improving joint health will likely expand, offering hope to patients seeking non-surgical solutions.
PRP Injection Therapy: Procedure and Benefits
Platelet-rich plasma (PRP) injection therapy is a treatment that involves using the patient’s own blood to create a concentrated solution of platelets. The process begins with drawing a sample of whole blood, which is then processed to isolate the platelet-rich plasma. This PRP is packed with growth factors and blood cells that are essential for healing. Once the PRP is prepared, it is administered through a targeted injection into the affected area, such as the knee joint where cartilage damage is present.
How PRP Injections Work in Knee Cartilage Repair
PRP injections are particularly effective for treating knee osteoarthritis, as the growth factors in the platelet-rich plasma stimulate the repair of damaged knee cartilage. The injection administration focuses on delivering the PRP directly into the joint, allowing the growth factors to work on regenerating tissue, reducing inflammation, and improving physical function. PRP injection therapy is often considered when other treatments, like corticosteroids or hyaluronic acid, have not provided sufficient relief. The use of autologous conditioned plasma—derived from the patient’s own blood—minimizes the risk of adverse reactions, such as blood clots or infection, which are more common with synthetic treatments.
The Role of PRP in Treating Conditions Beyond Osteoarthritis
In addition to knee osteoarthritis, PRP treatment has proven effective for conditions like tennis elbow and tendonitis. The therapy is also being explored as an alternative to more invasive treatments like bone marrow transplants for certain joint and bone conditions. PRP injections are increasingly preferred over placebo treatments due to their ability to deliver significant improvements in both pain and joint function. Randomized trials and clinical studies have demonstrated that PRP injections outperform placebo injections in terms of reducing pain and enhancing mobility, particularly in chronic conditions.
Understanding Insurance Coverage for PRP Treatment
When considering PRP therapy, one of the key questions patients ask is whether the treatment is covered by insurance plans. Unfortunately, most insurance providers still classify PRP injections as experimental or elective, meaning coverage is limited. However, as more clinical evidence emerges supporting the efficacy of PRP treatment, particularly in randomized trials, insurance companies may begin to offer coverage options for this therapy.
Overall, PRP injection therapy offers a promising, minimally invasive option for individuals dealing with chronic joint pain and soft tissue injuries. By leveraging the body’s natural healing capabilities, PRP treatment focuses on long-term recovery and improved quality of life for patients seeking non-surgical alternatives.
PRP Preparation and Injection Administration Techniques
The effectiveness of platelet-rich plasma treatment heavily depends on the preparation methods and the precise administration of the PRP injections. The process starts by drawing a sample of whole blood from the patient, which is then placed in a centrifuge to separate the blood components. During this step, the goal is to concentrate the platelet-rich plasma, ensuring a higher density of platelets and growth factors that play a crucial role in tissue regeneration and healing.
The Importance of PRP Injection Techniques
Proper injection administration is essential for maximizing the benefits of PRP therapy. The injection is typically guided by ultrasound to ensure accurate placement in the target area, such as the knee joint for osteoarthritis or the tendons in cases like tennis elbow. The focused delivery of autologous conditioned plasma directly into the affected tissue allows the growth factors to immediately begin their work in repairing damaged cells, reducing inflammation, and promoting the regeneration of knee cartilage and other structures.
PRP vs. Other Injection Therapies
PRP therapy stands out from other injection therapies, such as corticosteroids or hyaluronic acid, because it is autologous, meaning it uses the patient’s own blood. This approach reduces the risk of adverse effects like blood clots, infections, or allergic reactions. Moreover, while other treatments might provide temporary relief, PRP injections target the root cause by stimulating the healing of tissues. The use of PRP in regenerative medicine also offers advantages over treatments like bone marrow injections, as it is less invasive while still harnessing the body’s natural healing properties.
Clinical Outcomes and Efficacy of PRP Injections
Numerous randomized trials and clinical studies have supported the efficacy of PRP injections in improving physical function and reducing pain. For example, in treating knee osteoarthritis, patients have reported significant improvements in mobility and pain levels following multiple PRP injections. The treatment has also been effective for other musculoskeletal conditions, where the focus is on enhancing joint function and reducing the symptoms associated with degenerative conditions. As research continues, PRP therapy is expected to become a cornerstone in managing chronic joint and soft tissue injuries.
PRP Therapy Applications Beyond Arthritis
While platelet-rich plasma (PRP) therapy is widely recognized for treating knee osteoarthritis and joint pain, it is also increasingly used for a variety of other musculoskeletal conditions. PRP injections are commonly utilized in sports medicine to address soft tissue injuries like tendonitis, ligament sprains, and even chronic conditions such as tennis elbow. The growth factors in PRP promote the healing of damaged tissues, which can lead to faster recovery times and improved physical function. This regenerative approach has made PRP a popular choice among athletes and active individuals seeking effective treatment options that don’t require extensive downtime.
The Future of PRP in Regenerative Medicine and Orthopedic Surgery
PRP therapy is gaining traction in regenerative medicine as a non-surgical alternative for conditions that previously required more invasive procedures. For example, in orthopedic surgery, PRP is used to support recovery and enhance outcomes in treatments for cartilage defects, bone marrow issues, and joint repair. The potential of PRP to work alongside stem cell therapy in treating complex conditions is also being explored, offering new avenues for managing degenerative processes. Ongoing clinical studies and new research in journals like J Sports Med and J Cell Physiol highlight the evolving role of PRP therapy in both clinical and sports settings.
Practical Considerations: Insurance Coverage and Patient Accessibility
Despite its proven benefits, PRP therapy is still considered an experimental treatment by many insurance plans, meaning that coverage is limited. Patients considering PRP treatment should consult with their insurance providers to understand their options. Out-of-pocket costs can vary, especially if multiple injections are needed to achieve optimal results. However, the long-term benefits of improved joint function, reduced pain, and enhanced physical activity can outweigh the initial expenses for many patients.
The Growing Body of Evidence Supporting PRP Treatment
A growing number of randomized trials and systematic reviews continue to demonstrate that PRP injections offer significant improvements in pain relief and joint function, especially in comparison to placebo treatments. The use of autologous platelet-rich plasma from the patient’s own blood ensures a low-risk, high-reward approach to managing chronic conditions. Clinical outcomes show that PRP therapy is an effective treatment for not only knee osteoarthritis but also for a wide range of soft tissue injuries and musculoskeletal conditions.
Conclusion
As research progresses and more patients experience the benefits of PRP, it is expected that platelet-rich plasma therapy will continue to expand in use and accessibility. From treating symptomatic knee osteoarthritis to addressing sports-related injuries, PRP offers a promising, natural approach to regenerative medicine. Whether seeking relief from joint pain, improved mobility, or accelerated healing from injuries, PRP injections stand out as a versatile treatment option with long-term benefits for those looking to avoid surgery and enhance their quality of life.
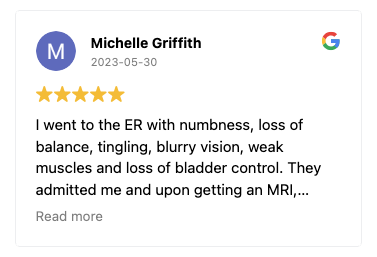
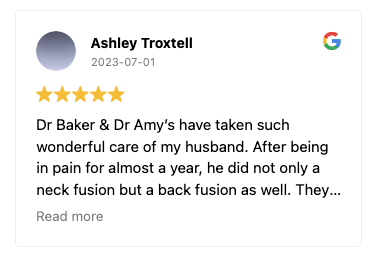
Dr. Abdul Baker - An Expert Neurosurgeon in Texas
Every neurosurgery has its complications; thus, a patient must choose the best neurosurgeon for himself. Dr. Abdul Baker is one of the most experienced and qualified neurosurgeons in Texas, treating patients for more than 16 years. People in Sherman, Plano, and nearby areas trust him for every kind of neurosurgery due to his surgical procedures’ 100% success rate. You may visit him if you need any consultancy or treatment regarding your brain and spine disorders.

Dr. Baker specializes in neurosurgery, neurosurgical spine surgery, neurotrauma, brain tumors, spinal tumors, and peripheral nerve damage treatment.