Bulging Disc Treatment
Welcome to our comprehensive guide on bulging disc treatments. In this exploration, we'll demystify the often-confused terms of disc protrusion, herniated, and bulging discs, and delve into their progression.
We'll uncover the root causes of a bulging disc, the role of physical therapy in treating herniated discs, and strategies for strengthening the spinal cord.
We will also navigate through various treatments, from conservative methods to advanced surgical options, and examine the place of alternative medicine in managing disc-related issues. Join us as we explore each facet to help you find relief and optimal spine health.
Is a Herniated Disc the same as a Bulging Disc?
Understanding the nuances between a herniated disc and a bulging disc is crucial for effective spine health management. While these terms are often used interchangeably, they describe different conditions.
Disc Protrusion
Disc protrusion is a broader term that encompasses various types of disc displacement, including both herniated and bulging discs. It refers to the condition where the disc extends beyond its normal boundary in the spinal column, potentially impacting nearby spinal nerves and causing pain.
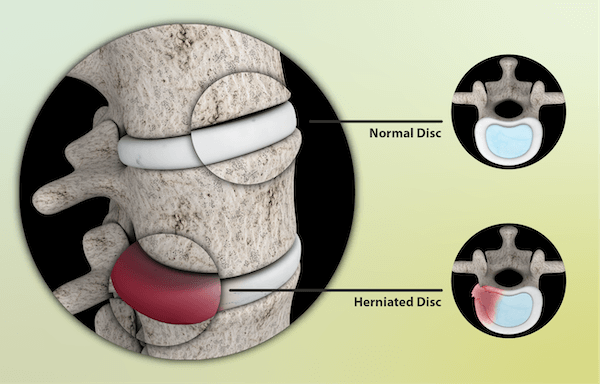
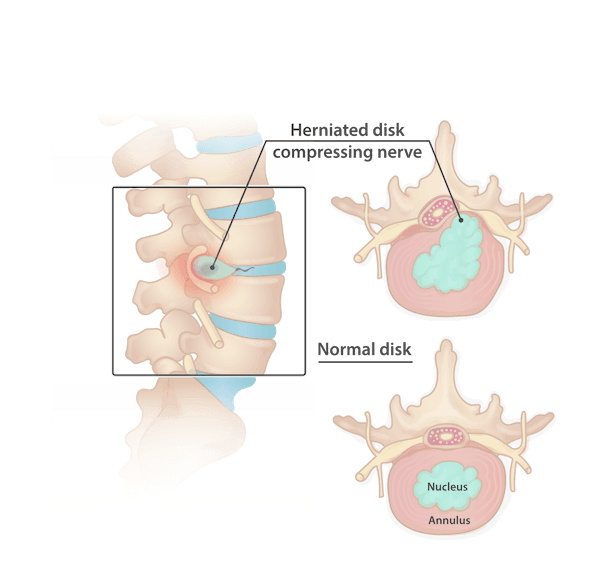
Herniated Disc
A herniated disc, also known as a slipped or ruptured disc, occurs when a tear in the disc's outer layer (annulus fibrosus) allows the inner material (nucleus pulposus) to escape.
This can lead to severe pain, often associated with nerve root compression. Symptoms may include sharp pain, muscle spasms, and in cases where the lumbar spine is affected, leg pain.
Herniated discs are more likely to cause significant nerve irritation due to the protruding portion of the disc material pressing directly against spinal nerves.
Bulging Disc
In contrast, a bulging disc is characterized by the disc's outer layer remaining intact, but the disc bulges out uniformly in all directions.

This condition is often part of the natural aging process and disk degeneration.
While bulging discs can cause discomfort, including back pain and neck pain, they don’t usually lead to the same level of nerve irritation or muscle weakness as herniated discs unless severe.
Bulging Disc Progression
Over time, a bulging disc can progress and potentially turn into a herniated disc, especially if subjected to continuous pressure or strain. The progression from a bulging to a herniated disc marks an escalation in severity, often necessitating more intensive treatments.
This could include physical therapy, spinal manipulation, or even epidural steroid injections for pain relief. In advanced cases where conservative treatments fail, a surgical procedure such as spinal fusion might be necessary to relieve pressure on the spinal cord or nerve roots and restore the spinal column's integrity.
Request an Appointment
Causes of a Bulging Disc
A bulging disc is a common spinal issue where a spinal disc extends beyond its usual space in the spinal column. This condition is often a result of a combination of factors affecting the spine's structure and function.
Degenerative Disc Disease
The primary cause of a bulging disc is degenerative disc disease. This condition arises from the natural aging process, where spinal discs lose their hydration and elasticity.
Over time, these discs, which act as shock absorbers for the spine, start to degenerate and weaken. This degradation makes them more susceptible to bulging, especially under the pressure of the upper body’s weight.
Physical Strain and Injury
Physical strain or acute injury can expedite the bulging of a disc. Activities that involve heavy lifting, bending, or twisting can put excessive pressure on the spinal discs, especially in the lumbar spine.
This undue strain can cause the disc to protrude beyond its normal boundary, leading to a bulging disc.
Lifestyle Factors
Lifestyle factors play a significant role in the development of bulging discs. Obesity, for instance, increases the load on the spinal column, particularly in the lower back, exacerbating the risk of disc protrusion. Similarly, smoking can affect disc health by reducing blood flow to the spine, hastening disc degeneration.
Poor posture, especially with too much bed rest or sitting for prolonged periods, can also contribute to disc issues.
It puts uneven pressure on the spinal column, leading to disc wear and tear. Inactivity further weakens the spinal muscles, reducing the support for the spinal column and discs.
Medical Conditions
Certain medical conditions like osteoarthritis can result from or contribute to a bulging disc. Osteoarthritis in the spine can lead to the breakdown of discs and vertebrae, increasing the likelihood of disc bulging.
Additionally, conditions that affect muscle strength and nerve function, like neuropathic diseases, can indirectly contribute to the risk of a bulging disc.
Age-Related Factors
As people age, the risk of developing a bulging disc increases. Aging leads to a natural decline in disc health, making them more prone to bulging.
This is compounded by age-related changes in muscle strength and bone density, which can affect the spine's ability to handle stress and maintain its structural integrity.
Treatment for a Bulging Disc
Treating a bulging disc effectively requires a multi-faceted approach, primarily based on the severity of symptoms, patient's age, and overall health. Here's a progression of treatments from initial conservative approaches to advanced treatments if conservative measures fail.
Initial Conservative Treatments
Medication:

The first line of treatment often includes over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen to relieve pain and reduce inflammation. For more severe cases, prescription pain medication, muscle relaxers to ease muscle spasms, and neuropathic drugs for nerve pain are considered.
Physical Therapy:
A cornerstone of bulging disc treatment, physical therapy involves exercises and hands-on therapy designed to relieve pressure on the spinal nerves and strengthen the muscles supporting the spinal column. This therapy aims to improve muscle strength, especially in the affected leg, and alleviate back pain.
Chiropractic Care:
Spinal manipulation by a chiropractor can relieve pressure on the spinal nerves, especially in cases of lumbar spine issues. This treatment is often effective for chronic low back pain.
Alternative Medicine:
Approaches like acupuncture appear to provide relief for some patients, especially in managing chronic pain and improving muscle strength and flexibility.
Heat and Cold Therapy:
Using cold packs initially helps reduce inflammation, followed by gentle heat applications to relieve muscle stiffness and pain.
Restricted Bed Rest:
While rest is important, too much bed rest can lead to stiff joints and weak muscles. Limited, comfortable rest combined with light activities is recommended.
Braces and Support Devices:
These can provide stability and help reduce pain, particularly when dealing with severe pain in the lumbar spine or cervical spine.
Advanced Treatments for Persistent or Severe Cases
- Cortisone Injections: Epidural steroid injections deliver cortisone directly to the inflamed area around the spinal nerves, providing longer-term pain relief.
- Spinal Decompression Therapy: This non-surgical treatment can alleviate symptoms by gently stretching the spine, relieving pressure on the spinal discs.
- Electrotherapy: Treatments like TENS, PENS, and rTMS can help manage pain by stimulating the nerves in the affected area.
- Surgical Options: If conservative treatments fail, surgical procedures such as spinal fusion, where a bone graft is used to join two vertebrae, or a discectomy, where only the protruding portion of the disc is removed, are considered. Surgical intervention is typically reserved for cases where the bulging disc causes severe pain, muscle weakness, or bowel control issues, or when neurological symptoms persist.
It's important to note that a patient's age, medical history, and the presence of conditions like disc degeneration or herniated disks can influence the choice of treatment. Magnetic resonance imaging (MRI) is often used to diagnose the condition precisely and guide treatment decisions. While severe pain or shooting pain in the back or leg may necessitate more immediate intervention, the goal of any bulging disc treatment is to relieve pain, relieve pressure on the spinal nerves, and restore the patient to normal activity levels as much as possible.
Minimizing the Risk of Relapse
After successfully treating a bulging disc, especially through non-surgical means, the focus shifts to minimizing the risk of relapse. A key component of this preventive strategy involves exercises that strengthen the muscles supporting the spine. These measures are crucial not only for those who have experienced a herniated disk or slipped disc but also for individuals with chronic back pain.
Strengthening the Spinal Support System
Core Strengthening:
A strong core is essential for supporting the spinal canal and alleviating pressure on the spinal nerves. Exercises like planks, pelvic tilts, and gentle yoga can strengthen core muscles without putting pressure on the spine.
Flexibility Training
Regular stretching exercises help maintain the flexibility of the muscles around the spinal column. This can prevent stiffness and reduce the risk of disc herniation. Incorporating yoga or Pilates can be particularly beneficial.

Posture Improvement
Poor posture, especially while sitting or standing, can exacerbate neck pain and back pain. Being mindful of posture, especially when working at a desk or using digital devices, is critical. Exercises that strengthen the muscles around the shoulder blades can help improve posture.
Aerobic Exercise
Low-impact aerobic activities like walking or swimming can increase blood flow to the spine and improve overall back health. This type of exercise is often recommended by physical therapists as part of initial treatment and ongoing maintenance.
Pain Management
For those who have undergone treatments like epidural steroid injections or used oral medications, continuing with a tailored pain management plan under the guidance of a pain doctor is important. This may include periodic check-ins and adjustments to the treatment plan.
Avoiding Activities that Increase Risk
- Limiting Heavy Lifting: Heavy lifting can exacerbate low back pain and increase the risk of a herniated disk. It’s important to use proper lifting techniques or avoid lifting heavy objects altogether.
- Avoiding Repetitive Strain: Repetitive motions that strain the back should be minimized. This includes being cautious about activities that involve twisting or bending, which can put undue stress on the spine.
- Recognizing Warning Signs: Numbness or tingling in the arms or legs can be a sign of nerve compression. Paying attention to these early warning signs and seeking medical advice can prevent a full-blown relapse.
- Alternative Therapies: For some, alternative therapies like acupuncture appear beneficial in maintaining spinal health and managing pain. These should be pursued under professional guidance.
Concluding Thoughts
Preventing a relapse of a bulging disc is as crucial as the initial treatment itself. By focusing on strengthening the spine through exercises, maintaining good posture, managing pain effectively, and being mindful of daily activities, individuals can significantly reduce the chances of re-injury. Speaking to an expert spine specialist surgeon like Dr. Baker can help you to understand a bulging disc.
Remember, only a small percentage of bulging disc cases require spinal surgery; with the right approach, many can maintain a healthy spine through non-surgical means. It's about creating a sustainable, spine-friendly lifestyle that nurtures your back and keeps it strong and supple for the long term.
Dr. Abdul Baker - An Expert Neurosurgeon in Texas
Every neurosurgery has its complications; thus, a patient must choose the best neurosurgeon for himself. Dr. Abdul Baker is one of the most experienced and qualified neurosurgeons in Texas, treating patients for more than 16 years. People in Sherman, Plano, and nearby areas trust him for every kind of neurosurgery due to his surgical procedures’ 100% success rate. You may visit him if you need any consultancy or treatment regarding your brain and spine disorders.

Dr. Baker specializes in neurosurgery, neurosurgical spine surgery, neurotrauma, brain tumors, spinal tumors, and peripheral nerve damage treatment.