Dr. Abdul Baker MD FAANS FACS
A Renowned Neurosurgeon With Exceptional Expertise
Based in Sherman and Plano, Texas, Dr. Abdul Baker holds the most trusted and experienced neurosurgeon spot. Before performing surgical procedures, he tests, diagnoses, and recommends the best course of action for a particular nerve and spine problem.
With his extensive training in neurosurgery, Dr. Baker uses cutting-edge diagnostic equipment and advanced treatment options. He gives you the best treatment for your pain because he is skilled in minimally invasive surgical techniques.
Dr. Abdul Baker is the surgeon you should trust for your brain, nerves, and spine disorders. He utilizes the latest robotic instruments to treat patients with brain and spinal diseases and problems. Henceforth, if you don’t want to take risks to your health, visit Dr. Baker for safe treatment.
He advises non-surgical solutions if they are more beneficial for the patients. However, if a patient needs a particular surgery, he should not be concerned because he is in the hands of the most experienced neurosurgeon in Texas.
Request an Appointment
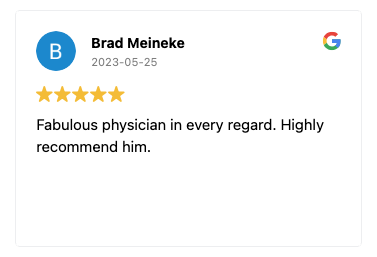
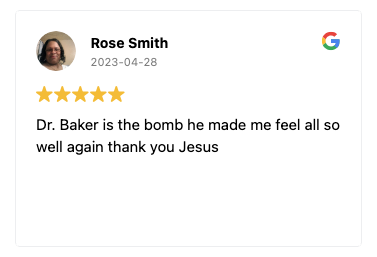
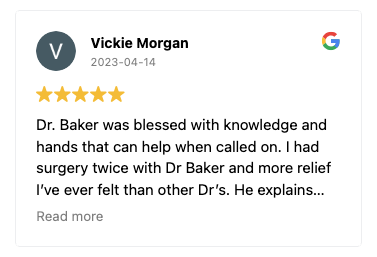
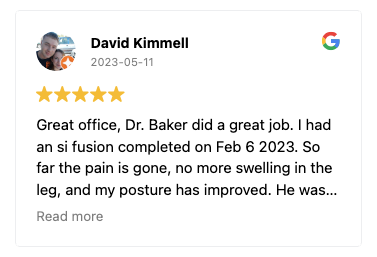
Patient Testimonials
The success stories of Dr. Baker’s patients are a testament to his exceptional care. Hear directly from those whose lives have been positively transformed through his expertise and compassion. Patient testimonials highlight the outstanding outcomes achieved under Dr. Baker’s guidance, illustrating the quality of care and the difference he has made in their neurological health.
Procedures Offered
Dr. Abdul Baker takes the time to evaluate each patient to determine the best possible treatment plan. Often there are non-surgical options, but if surgery is necessary, you are in experienced hands.
You will receive the greatest care possible, from robotic spine surgeries to artificial disc replacements. The fact that Dr. Baker performs minimally invasive spine surgery with a very high success rate is another factor that sets him apart as the top neurosurgeon.

Dr. Baker specializes in neurosurgery, neurosurgical spine surgery, neurotrauma, brain tumors, spinal tumors, and peripheral nerve damage treatment.